C.A.R.E Academy
SRC® SDoH INITIATIVE
Utilizing Social Determinants of Health to provide whole person care to achieve health equity in our communities with detoxification, inpatient, residential, and outpatient services, while ensuring we address health related social needs.

SDoH Areas of Focus
- Economic Stability
- Education Access and Quality
- Health Care Access and Quality
- Neighborhood and Built Environment
- Social and Community Context
What Is Whole Person Care?
Our initiative around whole person care is just that; treating the whole person instead of just treating substance use disorders or a single diagnosis. At Scottsdale Recovery, we treat the whole person. We know that long term recovery is depends on addressing not only health related social needs but physical health as well. Our positive outcomes on long term recovery depend on the intersection of many different factors including our patient’s ability to get to the doctor and access care. We also recognize the role of psychological, spiritual, and social health in overall wellness. Think of it as a one stop shop for healthcare.
Our patient-centered approach leverages a wide range of resources through our social determinants of health resource center to provide physical, behavioral, and social support. The goal is to achieve better care coordination, well-being, and health outcomes, all while incorporating the patient’s preferences, choices and ultimately achieving health equity.
Health Equity & Health Disparities
Health Equity
CDC defines health equity as the state in which everyone has a fair and just opportunity to attain their highest level of health.1 Health equity implies that everyone has a fair opportunity to achieve their full health potential and achieving health equity would mean the removal of “avoidable, unfair, or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, or geographically or by other means of stratification.”
Health Disparities
The U.S. Department of Health and Human Services defines a health disparity as “a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their: racial or ethnic group; religion; socioeconomic status; sex; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion.”
SDoH & HRSN
Social Determinants of Health (SDoH)
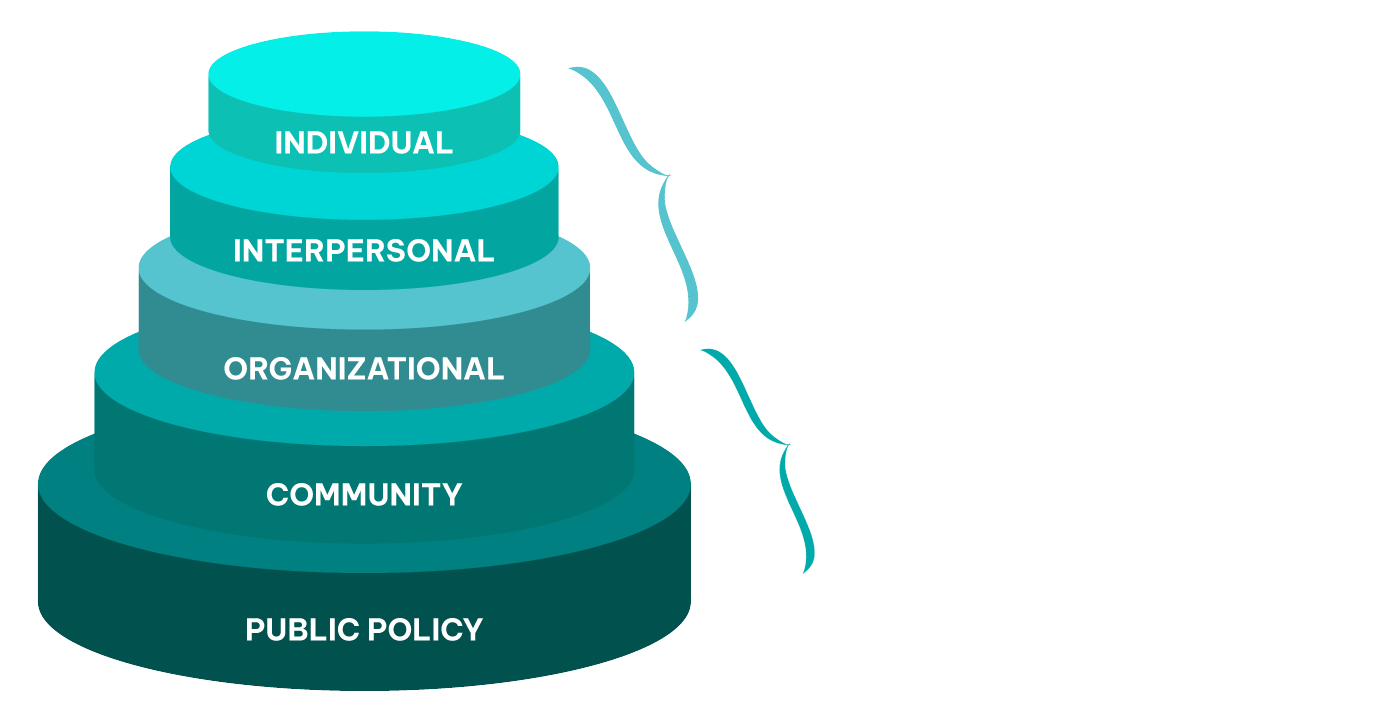
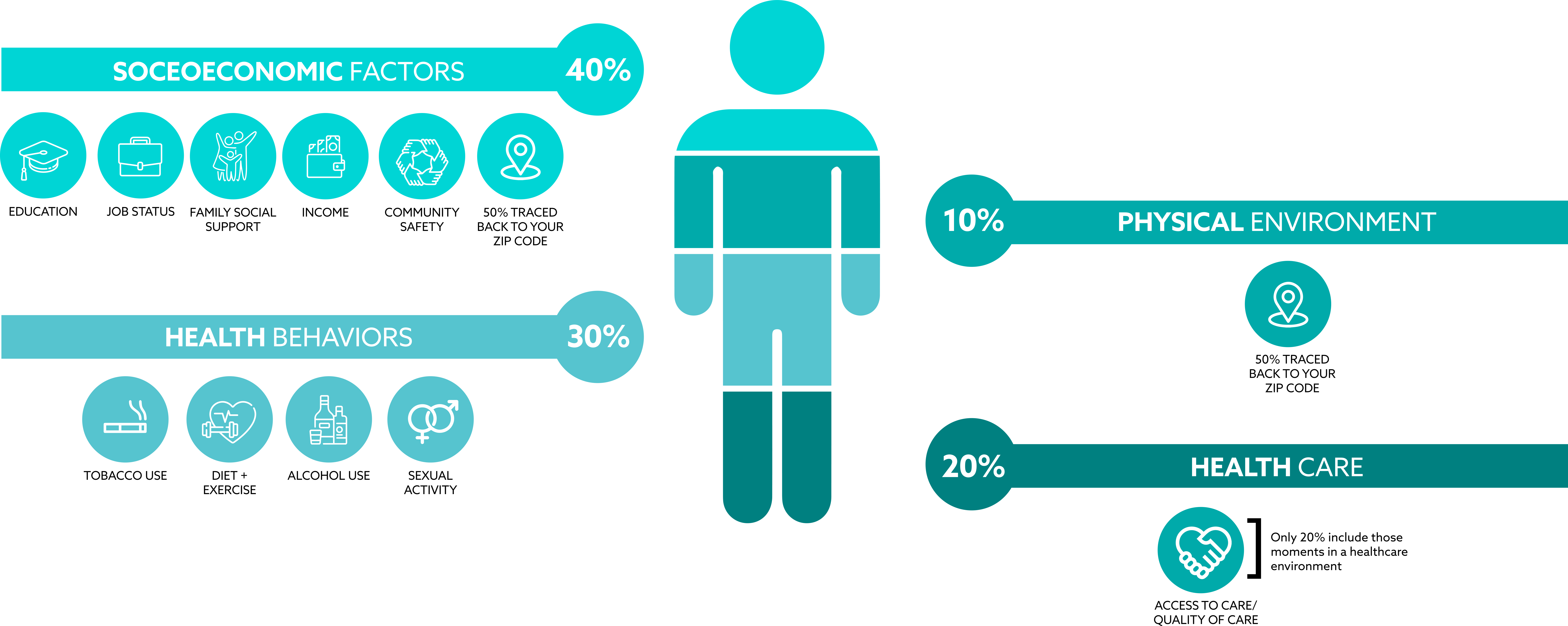
Social determinants of health (SDoH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality of life outcomes and risks. Disparities in these conditions contribute to health inequities.
The U.S. Department of Health and Human Services’ (HHS) Healthy People 2030 categorizes the social determinants of health into five groups:
- Economic Stability
- Education Access and Quality
- Health Care Access and Quality
- Neighborhood and Built Environment
- Social and Community Context
Consider looking into each of the five groups above to learn more about all the factors that can affect peoples’ lives, and to learn about CDC’s objectives in each area.
Health-Related Social Needs (HRSN)
While everyone has socially determined factors of health, some populations and individuals may have health-related social needs (HRSN) stemming from these factors. While SDOH are broader social conditions, HRSN are more immediate individual or family needs impacted by those conditions. They include housing insecurity, food insecurity, or lack of reliable transportation that can lead to decreased health and a lower quality of life.
Understanding SDoH and HRSN is Critical to Promoting Health Equity
Resources and Citations:
- NACDD has a Health Equity page that includes NACDD Action on Health Equity and other health equity resources, including a section specific to diabetes.
- CDC provides an extensive webpage on SDOH including research, data, and other SDOH tools.
- CDC also provides a guide to ten essential public health services and how they can include addressing SDOH inequities.
- The Health Equity Modifiable Slide Deck was created to support conversations between state health departments and partners working to promote the National DPP lifestyle change program. The slide deck’s content supports the potential for the National DPP lifestyle change program to help achieve health equity goals, reduce health disparities, and overcome health and economic social needs. This slide deck can be used as part of strategic conversations to obtain buy-in, create alliances, and initiate collaborations to improve health equity.
Information and Graphics: National Association of Chronic Disease Directors and Leavitt Partners. National Diabetes Prevention Program Coverage Toolkit, coveragetoolkit.org. June 2017. Prepared under Cooperative Agreement Number 5NU38OT000225-04, funded by the Centers for Disease Control and Prevention.
THE SRC® DIFFERENCE
WHY WE ARE
DIFFERENT
Longevity
One of the longest standing treatment centers in Scottsdale, serving the community.
Certified in Addiction
Medical Director is a licensed MD and certified as an Addictionologist by the American Board of Preventive Medicine.
Collaboration
Medical, Psychiatric and Clinical teams collaborate to provide individualized treatment plans addressing the 8 dimensions of wellness as well as psychiatric, emotional, mental, and physical well-being.
Family Workshops
Provide education and engage family members, spouses, and extended family in all aspects of the recovery process.
Alumni Program
(Scottsdale Recovery Continued)
Focuses on life after treatment and builds a community of sobriety and a place to always call home.
SERVICES
- Medication Assisted Treatment (MAT)
- Family Workshops
- Individual Counseling
- Group Counseling
- Peer Support
- Peer Support Certification
- Case Management Services
- Health-related Social Needs
- Independent Living Skills
- Workforce Development
- Psychiatric & Medical Services
- Outpatient Services
- Partial Hospitalization Program (PHP)
- Intensive Outpatient Program (IOP)
- Evening Intensive Outpatient Program (E-IOP)
- Re-Entry Program
- Right Restoration
- Fingerprint Clearance Cards
- Advocacy













